UnitedHealthcare (Optum) Coverage for Addiction: FAQs Answered
Getting rehab in Rhode Island without insurance is a huge financial burden. For instance, the daily costs for inpatient treatment can exceed $650 per day and give you a total bill of more than $55,000 for full recovery.
Now, if you don’t have an insurance plan at all or your plan doesn’t cover rehab, treating addiction will be 100x harder. And it’s also possible that you’ll keep delaying it till you have the funds, which will damage no one but you.
Luckily, UnitedHealthcare plans can save your 1000s in healthcare bills, including multiple treatment formats. But does UnitedHealthcare cover rehab in RI? Especially substance abuse rehab? If these questions are on your mind, we hear you.
This blog answers multiple questions regarding this insurance program, including the main one: Does UnitedHealthcare cover rehab in RI? So stick around a little longer, and we’ll clear as many of your doubts as possible.
Does UnitedHealthcare Cover Rehab in RI?
Lucky for you, UnitedHealthcare (UHC) covers drug and alcohol rehab in Rhode Island. The Affordable Care Act and federal parity laws require insurance providers to cover substance use disorder treatment just like other surgical and medical treatments.
Your UHC coverage for rehab in ID will typically include all steps, including medical detox, inpatient rehab, PHP, and IOP.
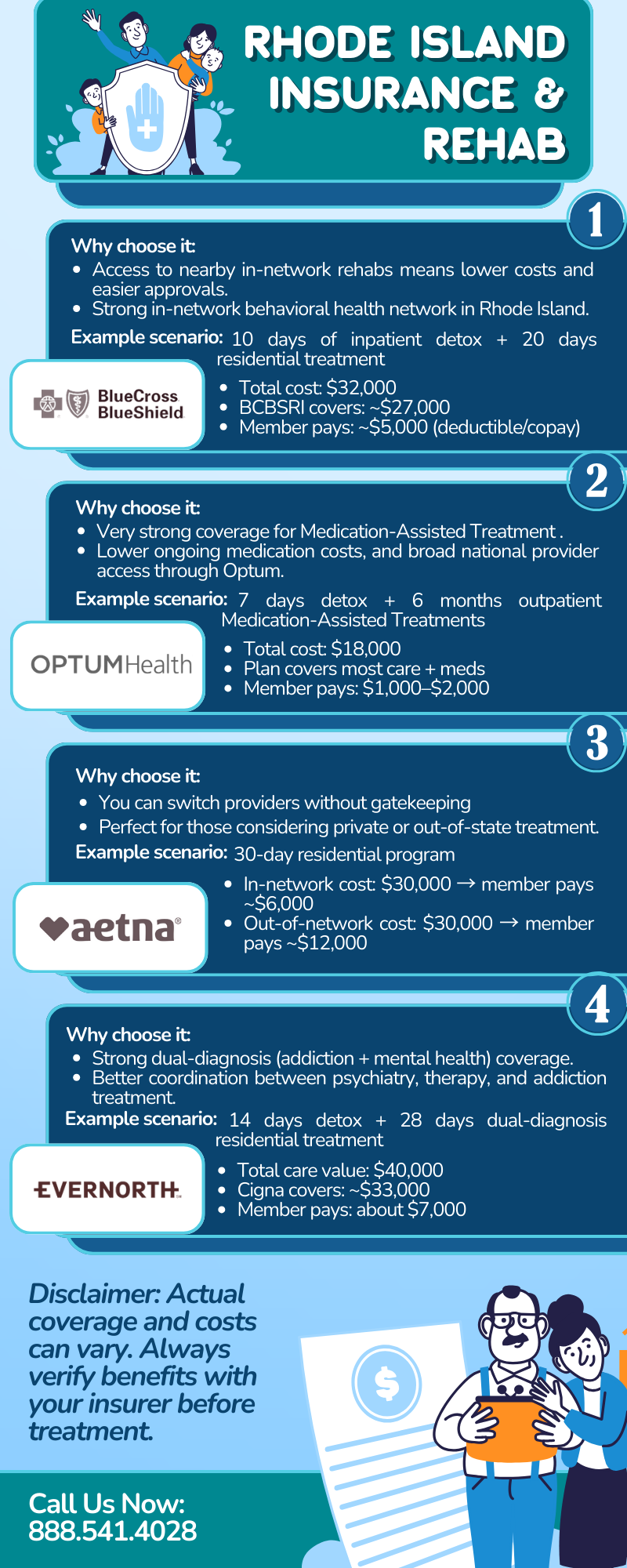
It’s worth noting that UnitedHealthcare operates across several plan types in RI. For example, it has commercial employer plans, marketplace plans, and the RIte Care (Medicaid) program.
And since the Ocean State has strict mental health parity laws, UHC is bound to ensure that your benefits for addiction treatment are no more restrictive than those for physical medical surgeries.
Also, like any other insurance program, your specific financial responsibility for a rehab will depend on your plan’s network status.
UHC maintains a robust network of local partners in Rhode Island. Staying in-network will make sure that UHC pays the maximum percentage of your treatment costs. But if you seek substance abuse or mental health rehab outside of the UHC network despite having its plan, you’ll face much higher out-of-pocket costs, or, in some cases, you’ll get no coverage unless it is an emergency admission.
Does My UnitedHealthcare Plan Cover Out-of-State Rehab?
UnitedHealthcare generally covers out-of-state rehab, but the bills you’ll pay will be influenced by your plan type. Sure, UHC is a national provider with a massive network, but many RI-specific plans (like RIte Care/Medicaid) prioritize local RI providers. So to avoid massive bills, always verify if the out-of-state facility you’re eyeing is registered with UHC before enrolling.
Let’s clarify it further.
If you have a UHC PPO plan, you can travel to a facility in another state. Still, the most cost-friendly rehab will happen if you choose an in-state provider.
On the other hand, if someone is on the standard RIte Care or Rhode Health Partners (Medicaid), coverage is stricter. These plans don’t cover you if you get rehab in another state unless the specific treatment is unavailable within Rhode Island or it is a life-threatening emergency.
How Do I Prove “Medical Necessity” to UnitedHealthcare for Substance Abuse Rehab?
You don’t do it; your doctor or the rehab center does. Medical necessity means that the level of care you’re seeking in rehab (such as inpatient stay) is the most appropriate option for your condition.
UnitedHealthcare (and its behavioral health arm, Optum) requires a clinical reason to pay for intensive services, such as inpatient detox.
The process is called Prior Authorization, and reputable centers like Rhode Island Addiction Treatment Centers have dedicated insurance specialists for this. They gather your medical history and symptoms to “make the case” to UHC.
And once they have a green signal, your treatment or admission process will start, depending on what the clinicians agree on.
What Will My Out-of-Pocket Cost Be in Rhode Island?
There’s no standard answer to this because what you pay for rehab besides your insurance depends on a few things. For instance, RIte Care (Medicaid) members pay $0 for treatment at state-approved facilities. On the other hand, commercial plan holders are asked to meet their deductible before insurance begins sharing the cost. And once you reach your out-of-pocket maximum, UHC clears the bills for remaining covered services on its set rate.
Can I Get Medication-Assisted Treatment Covered in RI?
Yes, UnitedHealthcare covers Medication-Assisted Treatment (MAT) in Rhode Island. In most cases, MAT is integrated into the standard healthcare system, and you don’t always have to go to a specialized “rehab” to receive it.
And under Rhode Island’s parity laws, UHC cannot make it harder for you to get addiction medications than it would be to get medication for diabetes or heart disease. Notably, most generic forms of Buprenorphine (a detox medicine) are classified as Tier 1 drugs and carry the lowest co-pays (sometimes as little as $0 to $10 per month).
Also, if someone requires Methadone, UHC covers the dosing at certified opioid treatment programs across the state.
What Happens if UnitedHealthcare Denies My Coverage?
In that case, you have a legal right to an appeals process because RI patients have some of the strongest mental health parity protections. If UHC denies your rightful insurance coverage for drug or alcohol rehab, the law makes sure that you aren’t stuck.
Most rehab facilities in RI will initiate an immediate review and speak to a UHC medical director to reverse the denial.
If that also fails, you move to a formal appeal, and because addiction is life-threatening, you rarely have to wait the standard 30-day window. An expedited appeal forces a quick turnaround, mostly within 24 to 72 hours.
Know Your Benefits and Make the Most Out of Them
You pay for insurance plans so they cover the basics for you when things get tough. If you have gotten addicted to a substance and want out of it, your UHC insurance might help you pay for rehab. So call your provider and make sure every dollar you pay benefits you when needed!