From Constant “On Guard” to Steadier Days: PTSD Outpatient Treatment in RI
“Trauma Changes The Way We See The World—But Healing Can Change It Again.”
At Rhode Island Addiction Treatment Centers, we often meet people who feel stuck in PTSD symptoms like flashbacks, nightmares, and constant “on guard” stress. In fact, 3.6% of adults had PTSD in the past year, and 6.8% have experienced it at some point in life.
The good news is that effective, evidence-based care exists, and it does not always require inpatient treatment.
In this guide, you will learn what a Trauma & PTSD Outpatient Program in RI is, who it helps most, what therapies work best, what a week can look like, and how to start with a clear plan you can follow.
What Trauma & PTSD Outpatient Program In RI Means In The Treatment Journey
A Trauma & PTSD Outpatient Program in RI offers structured, higher-support care while you stay in your own home. It can be a strong option when PTSD symptoms affect daily life, yet you can still remain safe between sessions.
This level of care often sits between weekly counseling and inpatient treatment. Because your needs can change over time, outpatient care can also serve as a “step-down” after a higher level, or a “step-up” if weekly therapy is not enough.
How Trauma & PTSD Outpatient Programs Fit The Care Continuum
A focused outpatient program targets the core patterns of PTSD, such as intrusion, avoidance, and hyperarousal. You receive frequent therapy contact, learn skills, and then practice them in real life while living at home.
Trauma guidelines also point to specific therapies that work best. A review of guideline recommendations notes that Prolonged Exposure (PE), Cognitive Processing Therapy (CPT), and trauma-focused CBT are strongly recommended treatments for adults with PTSD.
Typical Schedule In A Trauma & PTSD Outpatient Program In RI
Many outpatient and intensive outpatient programs are built around multiple sessions per week. For example, a six-day intensive outpatient PTSD program study describes large symptom reductions tracked through standard measures over follow-up.
In many programs, schedules can be offered in day or evening tracks. As your PTSD symptoms improve, the weekly hours may taper while your team builds a clear step-down and support plan.
Level Of Care | Setting | Weekly Hours (Typical) | Best For |
Weekly Therapy | Home | 1–3 | Mild symptoms, good stability |
Trauma & PTSD Outpatient / Intensive Outpatient | Home | 9–20 | Moderate to severe symptoms, safe at home |
Partial Hospitalization | Home | 20+ | High structure without overnight stay |
Inpatient | Facility | 24/7 | Acute safety risks |
Who Benefits Most From Trauma & PTSD Outpatient Program In RI
A Trauma & PTSD Outpatient Program in RI can help when symptoms disrupt sleep, work, relationships, or self-care, but you can still remain safe at home. This is especially important when you need more structure than weekly sessions provide.
At intake, we focus on safety and daily functioning. We also look at what triggers symptoms, what supports you already have, and what kind of schedule you can realistically attend.
Common Signs You May Need Trauma & PTSD Outpatient Care
You may benefit from this level of care if:
- Flashbacks or intrusive memories show up often and feel hard to control.
- Nightmares disrupt sleep several nights each week.
- Avoidance keeps you from people, places, driving routes, or work tasks.
- You feel constant hypervigilance, irritability, or startle responses.
- Weekly therapy helps insight, but symptoms still feel intense.
When Inpatient Or Higher Care Makes More Sense
A higher level of care may be safer if:
- You have suicidal thoughts with plan or intent.
- You are self-harming or having severe dissociation episodes.
- You cannot eat, sleep, or manage basic daily needs.
- Substance use is severe enough to require medical detox first.
If you are unsure, an assessment can clarify the safest starting point.
PTSD Symptoms And Conditions Treated In RI Outpatient Programs
PTSD symptoms are often grouped into clusters such as intrusion, avoidance, negative changes in thinking and mood, and hyperarousal. A good outpatient program addresses all clusters with trauma-focused therapy, not only general support.
Many people also carry more than one trauma, or more than one diagnosis. So we treat what is most active right now while also building stability skills for long-term recovery.
Core PTSD Symptoms Targeted In Treatment
Common targets include:
- Intrusion: flashbacks, nightmares, and unwanted memories.
- Avoidance: steering away from reminders and situations.
- Negative thoughts and mood: guilt, shame, numbness, low trust.
- Arousal: hypervigilance, anger spikes, sleep problems.
Co-Occurring Conditions Often Treated Alongside PTSD
It is also common to address:
- Depression linked to chronic stress and trauma impact.
- Anxiety disorders like panic and social withdrawal.
- Mild to moderate substance use used as a coping tool.
- Dissociation or emotional numbing patterns.
Types Of Trauma Commonly Addressed
Outpatient trauma work may focus on:
- Combat or military trauma.
- Sexual assault or domestic violence.
- Childhood abuse or neglect.
- Accidents, disasters, or sudden loss.
Evidence-Based Therapies In Trauma & PTSD Outpatient Program In RI
People often ask, “Will this actually work?”
Research and guidelines strongly support trauma-focused therapies, especially approaches that directly process trauma memories and trauma-related beliefs.
We also plan treatment in a practical way. That means you learn a skill, practice it between sessions, and then return to adjust what worked and what did not.
Prolonged Exposure (PE) Therapy
Prolonged Exposure (PE) helps you face trauma memories and avoided situations in a planned, safe way.
Guidelines recognize PE as a strongly recommended PTSD treatment.
In intensive outpatient formats for veterans, PE-based programs have shown strong retention and large reductions in PTSD symptoms, along with improvements in depression.
Cognitive Processing Therapy (CPT)
Cognitive Processing Therapy (CPT) focuses on “stuck points,” such as self-blame, guilt, or the belief that the world is never safe.
A guideline review also identifies CPT as strongly recommended for PTSD.
CPT can be delivered in standard weekly formats or in more intensive schedules.
Intensive outpatient options can increase momentum by keeping skills practice close together.
Trauma-Focused Cognitive Behavioral Therapy
Trauma-focused CBT combines skills training with focused work on trauma-related thoughts and feelings. It is also listed among strongly recommended PTSD treatments in the guideline review.
This approach can be especially helpful when anxiety and avoidance are driving daily limitations. It also supports clear homework, so you practice skills in real settings.
Group Skills And Psychoeducation
In outpatient programs, group work often adds strength and structure. Group sessions may include:
- Psychoeducation to explain why PTSD symptoms happen.
- Grounding skills for panic, flashbacks, and dissociation.
- DBT skills for emotion regulation and distress tolerance.
- Peer support that reduces isolation and shame.
What Your Week Looks Like In Trauma & PTSD Outpatient Program In RI
Structure helps reduce overwhelm. When you know what happens next, your brain can shift from survival mode into learning mode.
Also, frequent sessions reduce the “long gap” problem. Instead of waiting a full week to troubleshoot a hard moment, you can return quickly and adjust the plan.
Sample Weekly Schedule
A realistic week may look like this:
- Monday: 3-hour skills group (grounding, sleep, emotion regulation).
- Tuesday: Individual session (CPT or PE planning).
- Wednesday: 3-hour process group + trauma education.
- Thursday: 3-hour exposure practice or cognitive skills group.
- Friday: Review + optional family support meeting.
Program Length And Step-Down
Many outpatient and intensive outpatient tracks run about 6–12 weeks, depending on symptoms, safety, and progress. In some intensive models, the schedule is shorter but more concentrated, such as a 6-day intensive outpatient program.
Progress can also be tracked using standard tools like the PCL-5. The VA notes that a cutoff score around 31–33 can indicate probable PTSD in many samples, although cutoffs may vary by setting.
Proven Effectiveness Of Trauma & PTSD Outpatient Programs
Intensive outpatient PTSD treatment can show large symptom reductions. One study of a six-day intensive outpatient program found strong declines in PTSD symptoms from pre-treatment to follow-up, with large effect sizes reported at six months.
That same study reported that 52.4% no longer met PTSD diagnostic criteria after one month, and the reliable change analysis showed improvement for most participants.
Key Research Findings
Here are a few research signals that matter:
- Large symptom drops can occur in intensive outpatient formats, with effects maintained through follow-up.
- About 52.4% no longer met PTSD criteria one month after a six-day intensive outpatient program in one study.
- Reliable improvement was reported for 73.9% of patients on CAPS-5 in that study.
- Dropout from PTSD psychological therapy trials averages around 16% across studies, which is one reason strong engagement strategies matter.
Why Intensive Outpatient Can Help More Than Weekly Therapy
Intensive outpatient care can help because:
- Frequent practice builds skills faster.
- Rapid feedback reduces backsliding.
- Group momentum supports follow-through.
- Less time between sessions means less “forgetting.”
Research Snapshot Table:
|
Approach |
What It Helps With |
What Research Shows |
|
Trauma-Focused Therapy (PE, CPT, trauma-focused CBT) |
Core PTSD symptoms and trauma beliefs |
Strong guideline support for PE, CPT, and trauma-focused CBT |
|
SSRIs (medication) |
Symptom reduction for some people |
Sertraline response rates around 50–60% reported in a review, often used with therapy |
|
Intensive Outpatient PTSD Programs |
Faster momentum and high engagement |
Large symptom reductions and meaningful loss of diagnosis rates reported in studies |

Insurance Coverage For Trauma & PTSD Outpatient Program In RI
Coverage depends on your plan, network status, and medical necessity rules. Still, many people can use insurance for outpatient mental health services when documentation supports the level of care.
Because authorization rules vary, we recommend verifying benefits early. That way, you can start with fewer surprises and a clearer financial plan.
Questions For Your Insurer
Ask your insurer:
- Is this Trauma & PTSD Outpatient Program in RI in-network?
- Do I need prior authorization, and for how many weeks?
- Are psychiatry and medication visits billed separately?
- What paperwork is needed to prove medical necessity?
Choosing Your Trauma & PTSD Outpatient Program In RI
Program quality matters as much as program intensity. Look for true trauma specialization, not only general counseling.
Also, practical fit matters. The best program is the one you can attend consistently, because consistency supports progress.
Program Quality Checklist
Look for:
- Trauma-focused therapies like PE, CPT, or trauma-focused CBT.
- Licensed clinicians with PTSD training and supervision.
- Regular symptom measurement, such as PCL-5 tracking.
- Step-down and aftercare planning from the start.
Questions To Ask Programs
Ask:
- “How much of care is trauma-focused rather than general support?”
- “How do you track PTSD symptoms over time?”
- “What happens if I need a higher level of care?”
- “What does aftercare look like after discharge?”
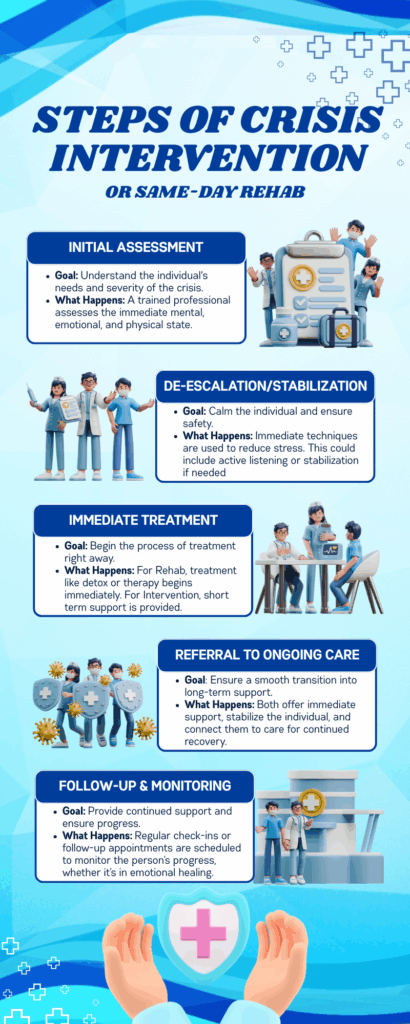
Getting Started With Trauma & PTSD Outpatient Program In RI
The first step is a confidential conversation. You do not need to have perfect words, because our role is to listen and guide the next steps.
After that, we complete an assessment, recommend the right level of care, and help you verify insurance and scheduling. This approach keeps the process clear and respectful.
Your Enrollment Path
Most people follow this path:
- Phone screening (about 15 minutes).
- Full assessment (about 60 minutes).
- Level-of-care match and scheduling.
- Day 1 orientation and safety planning.
Case Study
A veteran entered an intensive outpatient PTSD program that used Prolonged Exposure (PE) delivered in a concentrated schedule, supported by additional interventions. In that program, 80 veterans began treatment, and 77 completed it, showing a very high completion rate.
Across the program, participants showed large reductions in self-reported PTSD symptoms, as well as meaningful reductions in depression symptoms. After discharge, the veteran continued weekly therapy and kept using exposure practice, sleep routines, and grounding tools.
This continued practice helped maintain progress while returning to regular work and family responsibilities.
Conclusion
You deserve relief that fits your real life. You also deserve care that is proven, structured, and supportive. A Trauma & PTSD Outpatient Program in RI can help you face trauma safely, reduce daily symptoms, and rebuild trust in yourself again.
If you are ready to talk, call Rhode Island Addiction Treatment Centers at 888-902-3422. One conversation can clarify your options and your next steps.
Would you like help choosing the right level of care? Are you tired of carrying this alone? We are here to listen, answer questions, and help you move forward.